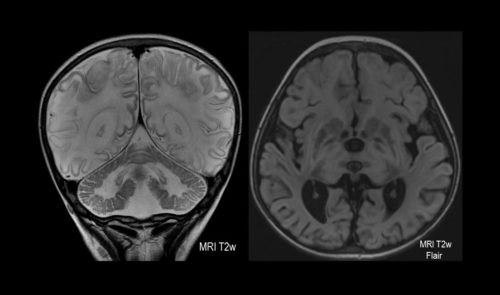
Cambridge-led trials spanning two decades have tested and led to the use of alternative, less-toxic maintenance treatments for anti-neutrophil cytoplasm antibody associated vasculitis (AAV), a group of rare but aggressive diseases that cause inflammation of blood vessels with the restricted blood flow leading to severe organ damage. Currently, 115,000 people are suffering from AAV across Europe and the USA, with at least 7,500 new cases diagnosed each year.
Cyclophosphamide is an effective immunosuppressant that was used widely to treat AAV; however, the drug is highly toxic and can cause bleeding from the bladder, infertility and various cancers. These side effects often necessitate reducing or stopping cyclophosphamide treatment, causing AAV to return in up to half of patients.
Research led by Cambridge University has optimised existing therapies and introduced new treatments for AAV, directly improving the survival, health and wellbeing of patients.
For instance, the results of the Cambridge-led PEXIVAS Study in 2020 led to an immediate change in practice, with physicians reducing steroid dose more rapidly across the NHS. This has reduced hospital readmissions by 20% and has become the new standard of care for patients with AAV. The optimisation of these conventional AAV therapies has seen first year fatality rates fall from 50% in 2007 to under 25% in 2020.
This improvement in therapies has produced more rapid and prolonged disease remission and reduced treatment-associated toxicities, thereby increasing patients’ quality of life and five-year survival.
Insights from this research have been incorporated into guidelines, the UK’s National Health System policy and healthcare provision for patients, and produced annual health-cost savings in the UK of £45 million.